Scientific Calendar November 2019 – DYSMORPHIC RBC
How can fluorescence flow cytometry (FFC) identify dysmorphic RBC?
A 30-year-old pregnant female was found to have microhaematuria and proteinuria during a routine obstetric evaluation. FFC examination found dysmorphic red blood cells (RBC) presenting as multiple populations of RBC. Further work-up led to a diagnosis of IgA nephropathy.
Haematuria is defined as the presence of RBC in urine. Causes for haematuria can be categorised into glomerular, i.e. arising from damage to the kidney, or non-glomerular causes. In glomerular haematuria, RBC morphology is disrupted by membrane damage as the cells pass through a damaged renal filtration system.
In FFC, they thus present as a population of a smaller volume than isomorphic RBC. Aside from IgA nephropathy, other causes can be hereditary nephritis or glomerulonephritis as well as benign familial haematuria.
Which statements are true for dysmorphic RBC?
They often vary in shape, sometimes with inner and outer vesicle-like protrusions.
They are typically smaller than isomorphic RBC.
Their presence indicates a glomerular bleeding source.
RBC can lose their shape when crossing the basement membrane of the glomerulus and during passage along the tubular system.
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
Scientific background
Haematuria is a common presenting feature of renal and urologic diseases. It is described as the presence of elevated numbers of red blood cells (RBC) in urine. The morphology of urinary RBC has been advocated as a valuable diagnostic tool to differentiate glomerular from non-glomerular causes of haematuria. In non-glomerular haematuria, RBC are mainly uniform in size and shape, thus named ‘isomorphic RBC’. In contrast to this, glomerular haematuria is characterised by an increased variety of RBC shapes and sizes, and such RBC are generally called ‘dysmorphic RBC’ [1].
The exact pathophysiological mechanisms that give rise to the wide range of morphological alterations in dysmorphic RBC are not yet completely understood. It is hypothesized that dysmorphic RBC are RBC which leaked through a damaged glomerulus. Mechanical influences such as the passage through the gaps in the glomerular basement and the continuous changes in tubular osmotic pressure and pH cause surface protein degradation, loss of membrane skeleton proteins, and haemolysis, resulting in glomerular bleeding of distorted RBC. It has also been shown that the haemoglobin content is greatly reduced in glomerular dysmorphic RBC [2].
Besides doughnut-shaped ring forms with smooth or wavy structures, acanthocytes are a special form of dysmorphic RBC. Acanthocytes may easily be recognised as ring forms with vesicle-shaped membrane protrusions or blebs, that point either toward the centre or outward, resembling ‘Mickey Mouse ears’. They represent a reliable and specific biomarker for glomerular disease [3].
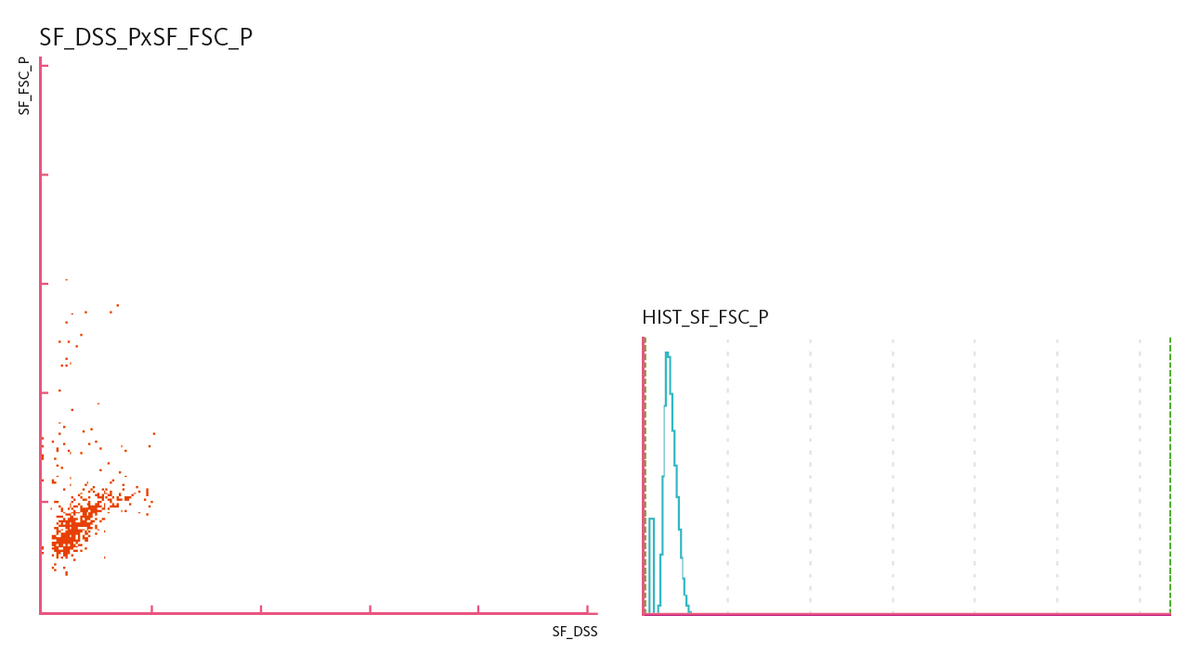
In clinical practice discrimination between glomerular and non-glomerular haematuria is often challenging. The reference method requires phase contrast microscopy and a skilled observer for the interpretation of results. State-of-the-art technologies such as fluorescence flow cytometry can facilitate screening for haematuria. If haematuria is detected, size and shape distribution of RBC are analysed automatically. Microscopy and confirmation of dysmorphic RBC can then be limited to specimens in which the morphology was assessed as abnormal.
IgA nephropathy
IgA nephropathy, also known as Berger’s disease, is an autoimmune disease and one of the common forms of glomerulonephritis. It occurs when immunoglobulin A (IgA) deposits build up in the kidneys and cause inflammation. This can damage the glomerular basement membrane, resulting in haematuria and proteinuria [4].
Scattergram and histogram
References
[1] European Urinalysis Group of the ECLM (eds. Kouri T et al.) (2000): European Urinalysis Guidelines. Scand J Clin Lab Invest. Vol. 60. Supplement 231.
[2] Crop MJ, de Rijke YB, Verhagen PCMS, Cransberg K, Zietse R (2010): Diagnostic Value of Urinary Dysmorphic Erythrocytes in Clinical Practice. Nephron Clin Pract. 115:c203-c212.
[3] Nagahama D, Yoshiko K, Watanabe M, Morita Y, Iwatani Y, Matsuo S (2005): A useful new classification of dysmorphic urinary erythrocytes. Clin Exp Nephrol. 9:304-309.
[4] Suzuki H, Kiryluk K, Nivak J, Moldoveanu Z, Herr AB, Renfrow MB, Wyatt RJ, Scolari F, Mestecky J, Gharavi AG, Julian BA (2011): The Pathophysiology of IgA Nephropathy. J Am Soc Nephrol. 22(10):1795-1803.